Navigating Sleep Study (Polysomnography) Options in Singapore
What is a Sleep Study?
A sleep study is a crucial tool for diagnosing sleep disorders. Whether conducted in a clinical setting or at home, a sleep study, also known as a polysomnography (PSG), plays a vital role in overall healthcare by providing insights into the impact of sleep on daily life.
In the busy, high-stress nation of Singapore, it is estimated that around 15% of adults suffer from insomnia, and 30% struggle with obstructive sleep apnea, a condition in which repeated breathing interruptions occur during sleep due to airway blockage.To discover the spectrum of sleep studies and the benefits involved, read on.

What is the Purpose of a Sleep Study?

As its name implies, a sleep study is a way to determine your sleep phases and cycles. It helps figure out if your sleep is being interrupted and what might be causing it.
- When you start to fall asleep, you first enter a phase known as non-rapid eye movement (NREM) sleep. In this phase, your brain starts to relax and slow down, which is tracked with a special test called an electroencephalogram (EEG).
- After about an hour or two in NREM sleep, your brain activity begins to increase again, signalling the start of the rapid eye movement (REM) sleep stage. During REM sleep, your eyes move quickly in different directions. This is also the time when most dreams happen.
- Throughout the night, you usually experience several of these sleep cycles, switching between NREM and REM sleep roughly every 90 minutes. However, if you have a sleep disorder, this natural cycle might be disrupted.
Types of Sleep Studies
In-Clinic Sleep Studies
In-clinic sleep studies are typically conducted by sleep technologists: healthcare professionals who specialise in diagnosing and treating sleep disorders. They come with professional equipment and immediate expert support, ensuring higher levels of accuracy in diagnosis.
These studies involve a comprehensive evaluation of various physiological parameters, including brain waves, eye movements, oxygen levels, heart rate, and muscle activity. Additionally, sleep specialists may conduct a physical examination to assess any external factors that could contribute to sleep disturbances.
1. Polysomnography (PSG)
- Comprehensive in-lab study for diagnosing various sleep disorders.
- Monitors brain waves, oxygen levels, heart rate, breathing, eye and leg movements.
2. Split-Night Polysomnography
- First part diagnoses sleep apnea, second part determines CPAP settings.
- Efficient for patients suspected of having sleep apnea.
3. CPAP Titration Study
- Determines the right air pressure setting for CPAP use in sleep apnea treatment.
- Combination of polysomnography with CPAP adjustment.
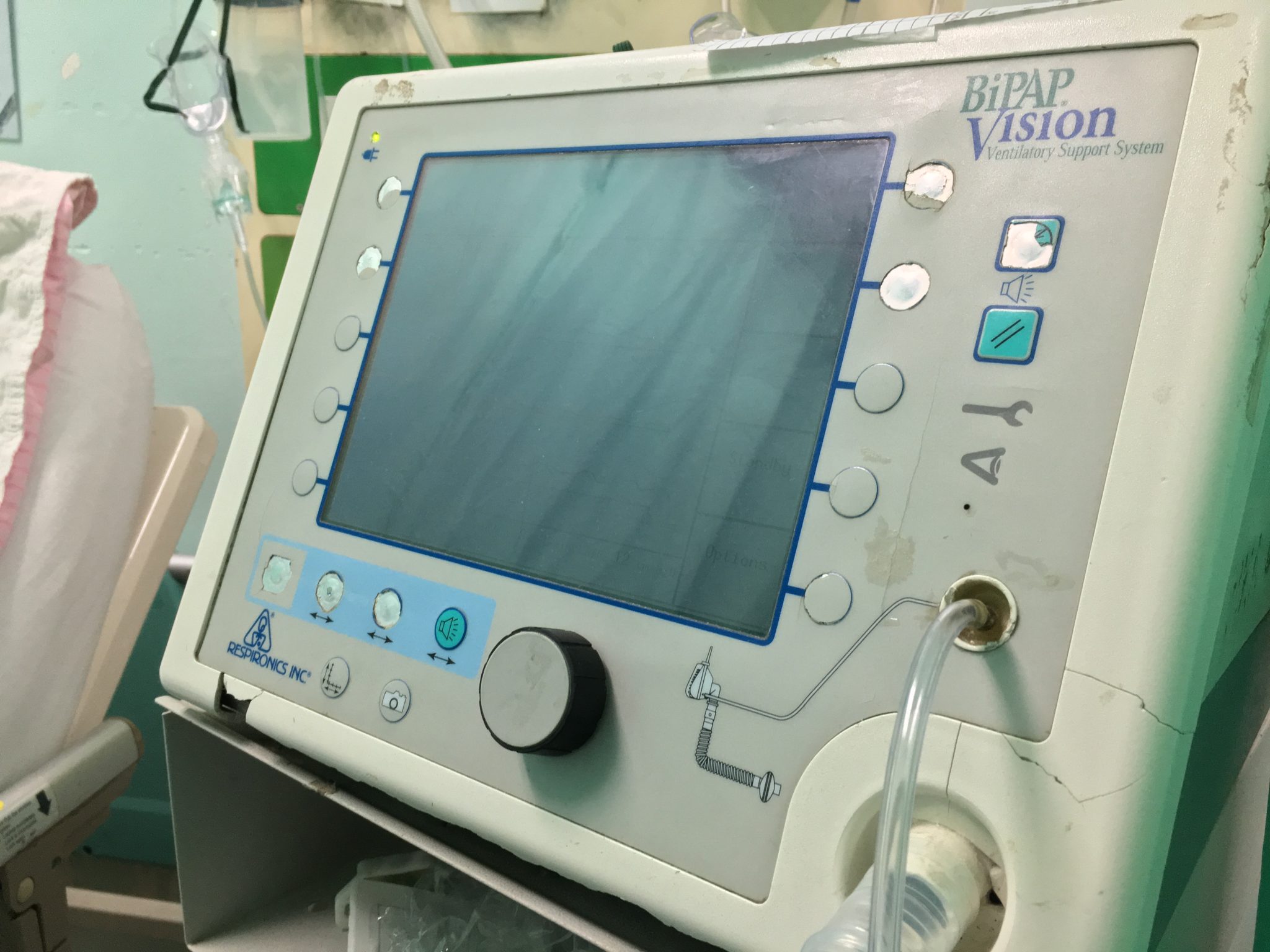
4. BiPAP Titration Study
- Aims to determine the optimal settings for BiPAP (Bilevel Positive Airway Pressure) therapy in treating sleep apnea.
- Similar to a CPAP titration study, but BiPAP provides two levels of air pressure: one for inhalation and a lower one for exhalation.
- Often recommended for patients who struggle with CPAP therapy or have other respiratory or cardiac conditions.
5. Adaptive Servo-Ventilation (ASV) Titration
- For patients with complex or central sleep apnea.
- Adjusts pressure based on patient’s breathing patterns.
6. Transcutaneous carbon dioxide monitoring
- A non-invasive method to monitor carbon dioxide levels in the blood during sleep studies.
- Helps in assessing the effectiveness of ventilation therapy, such as CPAP or BiPAP, in patients with sleep-disordered breathing.
- Important for detecting hypoventilation or nocturnal hypercapnia (high CO2 levels) in patients with conditions like COPD or neuromuscular diseases.
7. Maintenance of Wakefulness Test (MWT)
- A non-invasive method to monitor carbon dioxide levels in the blood during sleep studies.
- Helps in assessing the effectiveness of ventilation therapy, such as CPAP or BiPAP, in patients with sleep-disordered breathing.
- Important for detecting hypoventilation or nocturnal hypercapnia (high CO2 levels) in patients with conditions like COPD or neuromuscular diseases.
8. Multiple Sleep Latency Test (MSLT)
- Measures the speed of falling asleep in a quiet environment during the day.
- Primarily used to diagnose narcolepsy and idiopathic hypersomnia.
9. Full Electroencephalography (EEG) Sleep Study
- Involves the full electroencephalogram monitoring during sleep, providing a detailed brain wave activity assessment.
- Crucial for diagnosing sleep disorders that involve neurological issues, such as seizures during sleep or parasomnias.
- Offers a comprehensive evaluation of sleep stages and potential disruptions related to neurological conditions.
10. Oxygen Titration Study
- Determines the needed level of supplemental oxygen during sleep.
- Used for patients who require additional oxygen.
11. Actigraphy
- Uses a wearable device to estimate sleep patterns.
- Can be part of an in-clinic study or used for longer-term monitoring outside the clinic.
12. Electrocardiography (ECG or EKG)
- ECG records the electrical activity of the heart to identify any abnormalities that may affect sleep, such as arrhythmias.
- It helps in diagnosing conditions that can disrupt sleep, like sleep apnea, by monitoring for patterns indicative of cardiac stress or episodes of apnea.
13. Electro-oculography (EOG)
- EOG records eye movements to help identify the sleep stages, particularly REM (rapid eye movement) sleep, which is characterised by distinctive eye movements.
- It’s useful in diagnosing disorders like narcolepsy, which is marked by abnormal REM sleep patterns.
14. Electromyography (EMG)
- EMG evaluates electrical activity in muscles, identifying excessive movements or lack of muscle atonia during REM sleep.
- It aids in identifying sleep stages and diagnosing sleep-related movement disorders.
Home Sleep Apnea Testing (HSAT) or Out-of-Center Sleep Testing (OCST)
Home sleep studies offer a convenient way to assess and diagnose sleep disorders from the comfort of your own bed, and can be particularly useful for children or those uncomfortable in unfamiliar environments. At the moment, they are available only for the evaluation of OSA (Obstructive Sleep Apnea).
Type II Home Sleep Study
Type III Home Sleep Study:
Type IV Home Sleep Study
Oximetry
What Can a Sleep Study Diagnose?
- Obstructive and central sleep apnea.
- Narcolepsy.
- Insomnia.
- Disorders related to sleep behaviour, including sleepwalking.
- Periodic limb movement disorder, which encompasses restless legs syndrome.
- Night terrors, also referred to as sleep terrors.
- Nocturnal panic attacks.
- Sleep paralysis.
- Different kinds of seizures and epilepsy that occur during sleep.
- Other parasomnias and disruptive sleep disorders.
What Causes Sleep Disorders?
Psychological and Emotional Stress
- Anxiety or depression
- Stressful life events
- Grief or emotional trauma
Physical Health Conditions
- Sleep apnea (obstructive or central)
- Chronic pain conditions
- Hormonal imbalances (e.g., menopause, thyroid issues)
- Heart and lung diseases
Lifestyle and Environmental Factors
- Irregular sleep schedules
- Poor sleeping environment (noisy, too bright)
- Excessive use of electronics before bedtime
- High caffeine or alcohol intake
Neurological Disorders
- Narcolepsy
- Restless Legs Syndrome (RLS)
- Parkinson’s disease
- Alzheimer’s disease
Medications and Substances
- Certain medications (e.g., antidepressants, stimulants)
- Drug or alcohol abuse
- Withdrawal from sedatives
Aging
- Changes in sleep architecture
- Increased susceptibility to sleep disturbances
- Health conditions more common in older age
Genetic Factors
- Family history of sleep disorders
- Inherited conditions affecting sleep patterns
Disruption of Natural Sleep Patterns
- Shift work
- Jet lag from frequent travel
- Pregnancy
Sleep Study Procedure
In-Clinic Studies
Before the Procedure
- Meet Your Specialist: Personalised assessment during a one-on-one consultation.
- Prepare Yourself: Reduce intake of caffeine and alcohol; consult about medications.
- Your Sleep Diary: Maintain a detailed record of your sleep habits.
During the Procedure
- Getting Set Up: Technicians attach sensors, ensuring patient comfort.
- Your Sleep Space: A room designed to feel like a home bedroom.
- Gathering Your Sleep Data: Continuous monitoring of sleep patterns by clinic equipment.
After the Procedure
- Sensor Removal: Technicians carefully remove all equipment.
- First Insights: Immediate preliminary feedback provided.
Home Sleep Studies
Before the Procedure
- Consultation: Typically done remotely or through a preliminary visit.
- Preparation: Instructions on avoiding certain substances and maintaining medication routines.
- Sleep Diary: Advised to record sleep habits for better analysis.
During the Procedure
- Setup: Self-application of sensors with instructions focusing on comfort and correct placement.
- Your Sleep Space: The study takes place in your own bedroom.
- Data Collection: Sleep data recorded overnight by the equipment.
After the Procedure
- Sensor Removal: Guidance provided for safe and comfortable removal of equipment.
- Initial Insights: Feedback often communicated remotely or during a follow-up visit.
Follow-up Appointments (Applicable to Both In-Clinic and Home Sleep Studies)
- Understanding Your Sleep: Detailed discussion of the sleep report with the specialist.
- Planning Ahead: Development of a treatment plan or discussion of next steps based on findings.
Self-care and Maintenance (Applicable to Both In-Clinic and Home Sleep Studies)
- Adopt Healthy Sleep Habits: Guidance on improving sleep hygiene.
- Keep Track: Continued use of the sleep diary and adherence to any treatment plans.
What Does a Sleep Lab Look Like?
- Comfortable and Home-Like: Sleep labs are designed to mimic a bedroom setting, complete with a comfortable bed, soft lighting, and minimal medical equipment in plain sight, to make patients feel at ease as if they were in their own bedroom.
- Advanced Monitoring Equipment: Equipped with various technology, including polysomnography machines, each room features different sensors and equipment strategically placed to monitor sleep without being intrusive. This includes EEG electrodes for brain waves, ECG monitors for heart rate, and devices to measure breathing and oxygen levels.
- Quiet and Controlled Environment: The rooms are soundproofed to ensure a quiet environment, minimising external noises that could disrupt sleep. Temperature control is also maintained for optimal sleep conditions.
- Observation Facilities: Typically, there’s a separate observation area where sleep technicians monitor the patients remotely, ensuring privacy while still keeping a close eye on the data being recorded.
- Safety and Accessibility: Safety features are integrated, including emergency equipment and accessible designs for all patients, ensuring a secure environment during the sleep study.
- Connectivity for Analysis: The lab is equipped with networks and systems for real-time data capture and analysis, allowing sleep specialists to observe sleep patterns and disturbances as they occur.
Sleep Study Results
1. AHI
- Normal: AHI less than 5 events per hour
- Mild: AHI between 5 and 15 events per hour
- Moderate: AHI between 15 and 30 events per hour
- Severe: AHI greater than 30 events per hour.
2. Brain Waves and Eye Movements
3. Heart and Breathing Rate Changes and Changes in Blood Oxygen
4. Using PAP or Oxygen
5. Snoring and Other Noises
6. Limb Movements
7. Unusual Movements or Behaviours during Sleep
Benefits of Sleep Studies
1. Accurate Diagnosis
2. Personalised Treatment
3. Improved Health and Well-being
4. Reduced Risk of Other Health Issues
5. Better Daily Functioning
6. Understanding and Managing Your Condition
Am I a Good Candidate For a Sleep Study?
- Chronic and persistent snoring.
- Symptoms of sleep apnea, such as disruptive sleep patterns.
- Constant fatigue and lack of energy throughout the day.
- A history of stroke or other significant health conditions.
- Persistent muscle pain affecting sleep.
- Regular, severe headaches.
- Ongoing issues with acid reflux during the night.
- Sleep disturbances due to incontinence.
- The need to wear braces or other medical devices that affect sleep.
- Undergoing cancer treatment that impacts sleep quality.
- Seeking professional advice for sleep-related issues.

Common Sleep Disorder Treatments
Positive Airway Pressure (PAP) Therapy

CPAP (Continuous Positive Airway Pressure)
- Description: CPAP delivers a steady, continuous stream of pressurised air through a mask to keep the airways open during sleep.
- Use Cases: It is primarily used to treat Obstructive Sleep Apnea (OSA), a condition where the airway collapses or becomes blocked during sleep, causing breathing interruptions.
BiPAP (Bilevel Positive Airway Pressure)
- Description: BiPAP provides two levels of air pressure – a higher pressure when you inhale and a lower pressure when you exhale.
- Use Cases: BiPAP is used for treating Obstructive Sleep Apnea, particularly in patients who find it difficult to tolerate the continuous pressure of CPAP. It’s also beneficial for those with central sleep apnea, complex sleep apnea, or coexisting conditions like COPD (Chronic Obstructive Pulmonary Disease).
APAP (Automatic Positive Airway Pressure)
- Description: APAP automatically adjusts the pressure throughout the night based on your breathing patterns.
- Use Cases: APAP is primarily used for treating various forms of sleep apnea, including OSA. It is particularly useful for patients whose airway obstruction
Cognitive Behavioural Therapy for Insomnia (CBTI)
- CBTI is a structured program that helps people with insomnia identify and replace thoughts and behaviours that cause or worsen sleep problems with habits that promote sound sleep.
- Unlike sleeping pills, CBTI helps you overcome the underlying causes of your sleep problems.
- It typically includes strategies like establishing a regular sleep-wake schedule, limiting exposure to bed and bedroom for sleep only, relaxation techniques, and guidance on sleep hygiene.
- CBTI is highly effective and recommended as the first-line treatment for chronic insomnia.
Sleep Study Risks
Inconvenience: Overnight sleep studies require individuals to spend a night away from home in a sleep laboratory or clinic, which can be inconvenient for some individuals due to work, family, or other commitments.
Equipment Malfunction: Technical issues or equipment malfunction during the study may disrupt data collection and affect the accuracy of the results. Rare Complications: While rare, complications such as infection at the site of sensor attachment or adverse reactions to sleep study medications may occur in some cases. These risks are typically minimal but should be considered.Sleep Study Complications
Discomfort: Some individuals may experience discomfort due to the sensors and equipment attached during the study, leading to difficulty falling asleep or disrupted sleep patterns.
Anxiety: Being monitored while sleeping in an unfamiliar environment can induce anxiety in some individuals, potentially affecting the accuracy of the study results.Skin Irritation: Prolonged contact with adhesive patches or sensors may cause skin irritation or allergic reactions in sensitive individuals.
Sleep Study Cost in Singapore

In Singapore, a sleep study could cost you SGD 500-1,500. At home sleep kits are available from SGD 500 whereas in-hospital sleep studies may cost SGD 1,000-1,500.
For in-clinic studies, factors such as location, level of expertise, and the need for further testing can impact the overall sleep study cost. In some cases, private healthcare providers may charge higher prices compared to public settings. Insured patients may have costs covered with a doctor’s referral. For the most accurate and up-to-date pricing, consult with healthcare providers or sleep centres in Singapore. For financing options and a more detailed breakdown of costs, book a consultation with Nuffield today.Are There Subsidies for Sleep Studies in Singapore?
Why Choose Nuffield ENT For Sleep Studies?
At Nuffield ENT, we’re committed to giving you our best. Choose Nuffield for peace of mind, knowing you’ll get quality care every single time.
FAQ
1. How Common Are Sleep Studies?
Sleep studies are very common. Over 800,000 sleep studies were recorded in America in the year 2014.
2. How Long Does a Sleep Study Take?
A standard overnight sleep study typically lasts from 7 to 8 hours, reflecting a full night’s sleep duration. However, additional time may be required for preparation and equipment setup before the sleep study begins.
Certain studies like the Multiple Sleep Latency Test (MSLT) can take a full day to complete. They typically involve shorter nap periods during the day of around 20 minutes each.
3. What Not to do Before a Sleep Study?
Before a sleep study:
- Avoid caffeine and alcohol in the afternoon and evening to prevent sleep disruption.
- Do not take sleeping pills or sedatives 24 hours before the study for accurate results.
- Continue with your regular medications, except for sleep aids.
- Refrain from using hair sprays, oils, or gels, as they can interfere with the sensors.
4. Will I Be Watched During a Sleep Study?
Yes, a sleep technologist will monitor you throughout the night using a window or camera, depending on the facility in question. This ensures your safety and comfort.
5. What if I Can’t Sleep During a Sleep Study?
Whether or not you manage to fall asleep, you’ll still be providing valuable data for the study.
6. What Happens If I Need to Use the Bathroom During the Night?
Don’t worry, you can do so any time. If you need the bathroom, sleep technologists are prepared to quickly disconnect or unplug any necessary equipment. After you’re done, they will assist you in reconnecting or reattaching the equipment, ensuring uninterrupted monitoring for the remainder of the night.
7. Can I Do a Sleep Study at Home?
Yes, you can. However, sleep studies at home are currently available only for OSA (Obstructive Sleep Apnea) and tend to be less effective compared to clinical studies.
8. Do Sleep Studies Hurt?
No, sleep studies do not hurt. During a sleep study, sensors are attached to various parts of your body to monitor different physiological functions while you sleep. These sensors are painless and do not cause any discomfort.
9. Can You Eat Before a Sleep Study?
Generally, you can eat before a sleep study. However, it’s advisable to avoid caffeine after 5 pm to prevent it from affecting your sleep. For specific dietary guidelines, check with your testing centre.
10. Can I Bring My Own Pillow or Blanket to a Sleep Study?
Yes, you are usually allowed to bring your own pillow or blanket to a sleep lab or study for comfort. However, do check with the sleep centre beforehand to ensure that any personal items you bring comply with their hygiene and safety protocols. Some sleep centres may provide pillows and blankets for your use during the study.
11. What If I Experience Anxiety or Discomfort During the Sleep Study?
If you experience anxiety or discomfort during the sleep study, inform the sleep technologist immediately. They are trained to address such concerns and can provide reassurance or make adjustments to ensure your comfort throughout the night. Additionally, many sleep centres offer amenities or relaxation techniques to help you feel more at ease during the study.
12. Can Someone Be With Me for the Sleep Study?
It depends. While it’s generally more common for children or individuals with special needs to have a companion, most centres typically do not permit companions for adults in order to ensure the accuracy of data collection. It’s important to verify the specific policy of your sleep centre beforehand.
13. When Will I Receive My Results For the Sleep Study?
Sleep study results are usually provided within one to two weeks after the study. The data collected is analysed by a sleep specialist, who then prepares a report. This report is typically reviewed with you during a follow-up appointment with your doctor or sleep specialist.
Medical References
Aucar, N., Fagalde, I., Zanella, A., Capalbo, O., Aroca-Martinez, G., Favre, G., & Musso, C. G. (2023). Nocturia: its characteristics, diagnostic algorithm and treatment. International Urology and Nephrology, 55(1), 107-114. https://doi.org/unisimon.edu.co
Fonseca, P., van Gilst, M. M., Radha, M., Ross, M., Moreau, A., Cerny, A., … & Overeem, S. (2020). Automatic sleep staging using heart rate variability, body movements, and recurrent neural networks in a sleep disordered population. Sleep, 43(9), zsaa048. https://doi.org/10.1093/sleep/zsaa048
Lee, Y. Y., Lau, J. H., Vaingankar, J. A., Sambasivam, R., Shafie, S., Chua, B. Y., … & Subramaniam, M. (2022). Sleep quality of Singapore residents: findings from the 2016 Singapore mental health study. Sleep Medicine: X, 4, 100043.
Lombardo, R., Tubaro, A., & Burkhard, F. (2020). Nocturia: the complex role of the heart, kidneys, and bladder. European urology focus. https://doi.org/10.1016/j.euf.2019.07.008
Raut, A. D., & Dixit, B. (2020). Sleep Apnoea Disorder: A Review. European Journal of Engineering and Technology Research, 5(3), 339-342. Retrieved from ej-eng.org
